Promising Research Promotes Hope Among Veterans with Moderate to Severe TBI
Categories: Living with Brain Injury, Research
By Adam S. Hoffberg, MHS, and Lisa A. Brenner, Ph.D., ABPP-Rp, Rocky Mountain Mental Illness Research Education Clinical Center for Suicide Prevention
Traumatic Brain Injury and Suicide Risk
Among U.S. military personnel injured during Operation Enduring Freedom and Operation Iraqi Freedom, 10 to 20 percent sustained traumatic brain injuries (TBIs). TBIs are injuries caused by sudden trauma to the brain, such as a person’s head being struck by an object or a dramatic change in air pressure following explosions. Although the vast majority of TBIs are classified as mild, more than 40,000 service members have sustained moderate to severe TBIs since 2000 (DVBIC, 2018). While research has shown that veterans with a history of TBI are significantly more likely than other veterans to die by suicide (Brenner et al., 2011), a developing line of research offers promise that hopefulness can be increased among at-risk veterans with living with TBI.
The Original Australian Trial
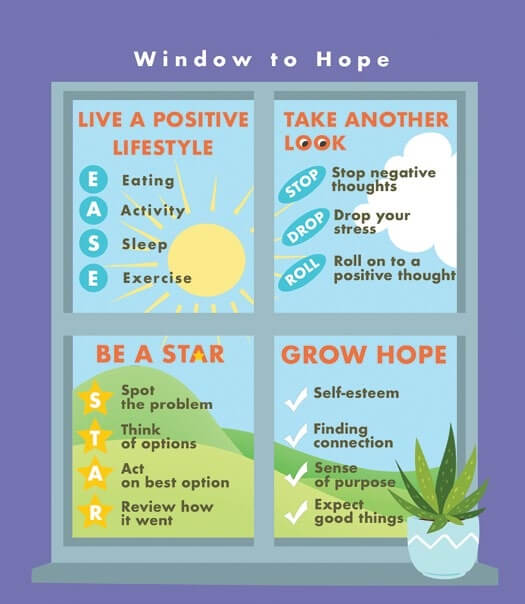
Before 2011, no studies looked at specific treatments to prevent suicide among adults with TBI (Bahraini et al., 2013). Grahame Simpson, Ph.D., and colleagues from Australia recognized a need to fill this gap and developed and tested a psychotherapeutic intervention called Window to Hope (WtoH). Based upon previous research suggesting that hopelessness is a strong predictor of who is likely to die by suicide and reducing hopelessness can reduce the risk of suicide, Simpson and colleagues focused on finding ways to increase hope (Beck et al., 1985; Simpson and Tate, 2002). The WtoH treatment is a ten-session program conducted in small groups that incorporates principals from cognitive behavioral and problem-solving therapies. Findings from the initial study demonstrated that it was possible to reduce hopelessness among adults with severe TBI (Simpson et al., 2011).
Adapting the Window to Hope Program for Veterans
Based on the need for treatments for veterans with TBI, Colorado researchers at the Department of Veterans Affairs (VA) Rocky Mountain Mental Illness Research Education & Clinical Center (MIRECC), led by Lisa A. Brenner, Ph.D., collaborated with Dr. Simpson to see if an approach similar to the one he pioneered might be able to reduce hopelessness among those seeking care in the VA.
The first step in this line of work was to adapt Dr. Simpson’s program to apply to U.S. Veterans. The team assembled a stakeholder panel that included experts in TBI and mental health, including those living with TBI. The panel unanimously agreed on a number of changes to the Australian model. Some were simple changes, like inserting the U.S. food pyramid in place of its Australian counterpart, while others were more substantive, such as modifying the manual to include “tactical breathing,” a type of deep breathing that U.S. service members are taught to use, instead of the original breathing exercises designed for use by Australian civilians.
The next step was to test the revised program among U.S. veterans with moderate to severe TBI. The pilot study was carried out with four different groups of veterans. Results suggested that the revised program was indeed feasible to implement within a Veterans Health Administration (VHA) setting as well as acceptable to those seeking care within VHA. Most encouraging were the comments from the veterans enrolled in the study, several of whom reported that the program did indeed help them build hope. In 2014, the group published a report in the journal Brain Injury describing this process (Matarazzo et al., 2014).
Second Trial Confirms Positive Impact of Window to Hope
The team then engaged in a randomized clinical trial designed to test the efficacy of the intervention to reduce hopelessness among veterans. Brenner and colleagues randomized 44 veterans, each with moderate to severe TBI and moderate to severe feelings of hopelessness. To evaluate whether the treatment worked, the researchers measured veterans’ feelings of hopelessness, depression, and thoughts of suicide at the beginning, middle, and end of the six-month enrollment period.
Participating in WtoH resulted in a reduction of hopelessness and depressive symptoms among veterans with TBI, and the favorable results were recently published in the Journal of Head Trauma Rehabilitation (Brenner et al., 2018). This rare replication of a psychological trial – with a different sample of participants, in a different country, and with different clinicians – increases the likelihood that changes observed among the participants were due to their participation in the intervention. Brenner and Simpson are now exploring strategies to provide and further evaluate this intervention to an even broader audience.
This article originally appeared in Volume 12, Issue 2 of THE Challenge! published in 2018.
