An Overview of the Best Practice Guidelines for Probationers with Brain Injury
Categories: ACBIS Insider
By: Molly Standeven and Kim Gorgens
Research has consistently demonstrated an over-representation of brain injury (BI) history (i.e., traumatic brain injury and acquired brain injury) among individuals who are involved in the criminal justice system (Gorgens et al., 2021, Shiroma et al., 2010). In community corrections specifically, 47% of individuals on probation report a significant history of BI (Gorgens et al., 2021).
These individuals have higher rates of behavioral health conditions and felony convictions. They also have lower rates of successful probation completion and are significantly more likely to reoffend (Gorgens et al., 2021). In community corrections, the cognitive and psychosocial consequences of injury may present as non-compliance and poor engagement, both of which increase the risk of probation failure (McMurran & Theodosi, 2007). In fact, these individuals have higher rates of behavioral health conditions and felony convictions and are more likely to be determined to be “high risk” by their probation officers. They also have lower rates of successful probation completion and are significantly more likely to reoffend (Gorgens et al., 2021).
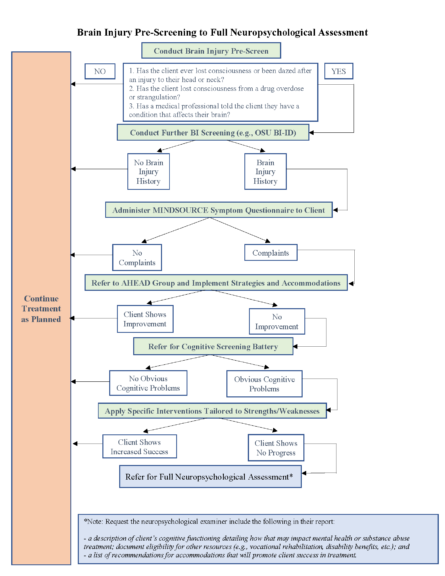
This article provides an overview of the recently completed Best Practice Guidelines for Supervising Probationers with Brain Injury, which outlines suggestions for the identification and management of BI and are grounded in the Colorado Brain Injury Model. The goal of the guidelines is to support probation officers in managing this high-need population and to promote self-advocacy among individuals on probation so that the burden of care is reduced for probation officers.
The Colorado BI Model has four aims: screening justice-involved individuals to identify a reported history of BI and assessing gross cognitive function, making referrals for care coordination, delivering strategies and self-advocacy training to individuals with BI, and building a knowledge base among criminal justice professionals and mental health professionals.
Screening
Traditional predictors of recidivism include substance abuse, involvement with criminal peers, exposure to violence, mental illness, and lack of treatment compliance (Blonigen et al., 2017; Hong et al., 2013; Kopak et al., 2016), all of which are overrepresented among probationers with BI history. Thus, screening for a history of BI in community corrections is imperative given the high stakes of poor outcomes for individuals in the community and the risk of BI symptoms being misinterpreted as behavioral issues. Screening for psychosocial and cognitive complaints ensures that the therapies and services delivered are modified for maximum impact.
The gold standard for the identification of BI and cognitive deficits is a medical record review and full neuropsychological examination. However, this is rarely feasible in community corrections due to limited time, budget constraints, and limited access to trained professionals. Instead, simple screening tools can be used by trained probation officers to identify significant self-reported BI history, cognitive dysfunction, and psychosocial vulnerabilities with minimal cost, time, and training necessary. At present, a structured clinical interview, or an interviewer-administered questionnaire, is a valid, near gold-standard for retrospective BI assessment (Corrigan & Bogner, 2007). The Ohio State University TBI Identification Method – Revised (OSU-BI-ID; Corrigan & Bogner, 2007) is unique in that it has been validated for use in correctional settings. The OSU TBI-ID is a standardized interview procedure for eliciting a person’s lifetime exposure to TBI through a three-to-five-minute structured interview. The OSU TBI-ID-Revised assesses three different domains: first injury, worst injury, and multiple injuries (Glover et al., 2018). In situations where there is too little time for the OSU-BI-ID, probation professionals can use the three pre-screen questions reflected on the “Brain Injury Pre-Screening to Full Neuropsychological Assessment Algorithm”:
- Have you ever lost consciousness or been dazed after an injury to their head or neck?
- Have you lost consciousness from a drug overdose or strangulation?
- Has a medical professional told you that you have a condition that affects your brain?
Referral
If a significant report of BI is identified during the screening process, probation officers can make community referrals. Preliminary data suggest that persons connected to resources through an identification and referral process show a reduction in recidivism and increase in community productivity (i.e., successful employment, volunteer work, training; Nagele et al., 2018). To find resources by state, probation department professionals can access the Brain Injury Association of America.
In these cases, the probation officer can also refer the probationer to a local or virtual Achieving Healing Through Education, Accountability, and Determination (AHEAD) group. The AHEAD group helps probationers understand brain injury and how they can ask for the support they need to be successful. The AHEAD groups are designed to be flexible, require minimal resources and time, and can be easily implemented. All group materials and facilitator resources are provided through this website: https://mindsourcecolorado.org/ahead/.
Strategy and Self-Advocacy
Among justice-involved populations, BI is associated with cognitive complaints and complex needs (O’Rourke et al., 2018) that can make managing supervisees and tracking progress more challenging for probation professionals. Implementation of simple, low-cost strategies in everyday interactions with supervisees can help reduce the burden on probation officers.
If the probationer screens positive for a significant reported history of brain injury on the screening interview, the probation officer can use a self-report symptom questionnaire or cognitive screening tool to identify cognitive and emotional complaints as well as difficulties in daily functioning (i.e., MINDSOURCE Symptoms Questionnaire). If the probationer complains of problems in any of the impairment areas (attention, delayed processing, emotional, inflexibility, inhibition, language, memory, organization, physical, and sleep), the MINDSOURCE Symptom Questionnaire website will generate an email to the probation officer with a customized strategy booklet and tip sheets for individuals on probation. These materials are designed to promote self-advocacy. The probation officer and probationer should work together to implement the strategies and accommodations recommended in these materials.
These Best Practice Guidelines for Supervising Probationers with Brain Injury aim to become a standard protocol that can be easily integrated into an existing intake workflow, minimizing demand on probation officers, and utilizing few resources.